by Sharon Joag, MSW, LSW
What is the first image you have when you think about Post Traumatic Stress Disorder? If you are like me, the first thing that pops into my head is a war veteran; and someone who has been through something that induces major trauma, sometimes lasting for a lifetime.
But what about those who have undergone major surgery? Although much less talked about, trauma from surgery has now become a global public health crisis. Globally, 310 million major surgeries are performed every year, and of those, 40-50 million surgeries are performed in the US (Dobson, 2020). From the moment a patient is given a diagnosis the black cloud of imminent surgery looms ahead. First, the anxiety sets in, and the rumination on the actual surgery, what it entails, what exactly will happen in the operating room. Questions in the minds of patients. “Will I feel anything while undergoing surgery? Will anesthesia work? What is going to happen after surgery?”
Doctors typically do not and cannot always talk to a patient about every single minute detail of a surgery. Surgeons can only provide an overview of a surgery, but the details are vague and sometimes unknown, even to the surgeon, until the surgery is actually underway. This uncertainty creates a milieu of confusion, and unhealthy rumination on all that could potentially go wrong, culminating in a deep anxiety and post-surgical depression that can last for months or years after the surgery, inevitably aiding in extending the recovery time of a patient who has undergone a major surgical procedure.
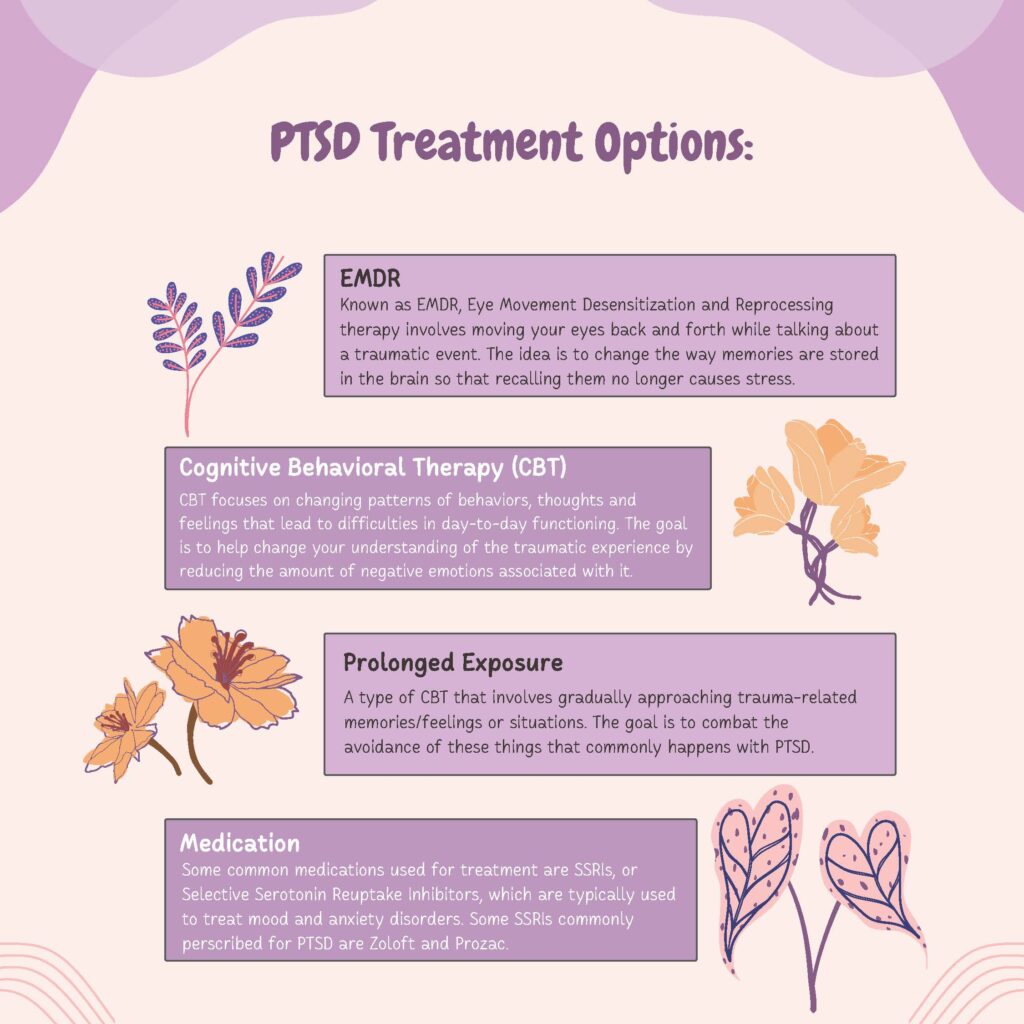
These ruminating thoughts can be overwhelming to an individual. Having regular therapy appointments to monitor an individual’s thought processes, and talk through some of these traumatic future events, especially a planned surgery is important in helping patients find tools that they can use to decrease stress levels, understand their thoughts, and find ways to manifest optimal mental health.
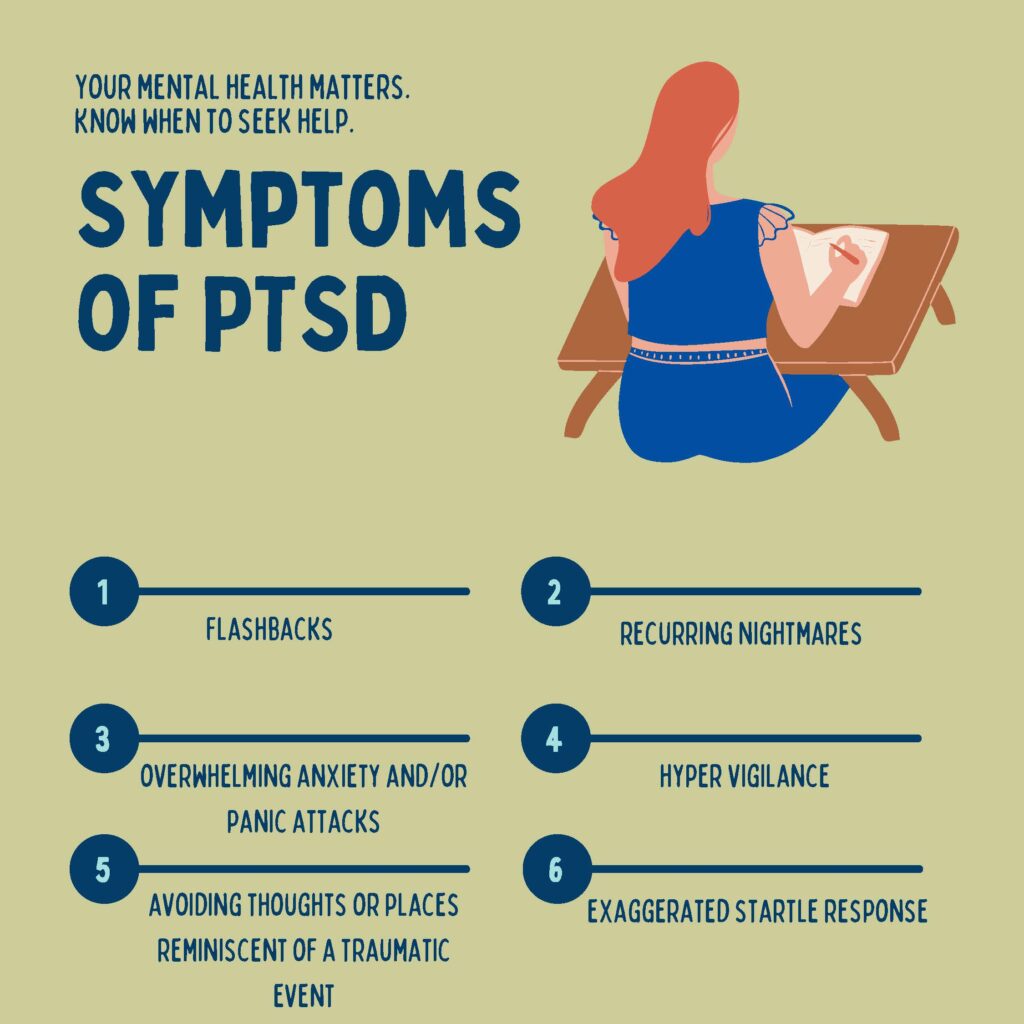
Many people suffer tremendously pre, peri and post surgically with anxiety and depression. Major surgeries such as surgery to remove cancer (breast, a portion of the esophagus, stomach or colon). The physical changes that a person has to endure post-surgery takes a toll on the psyche. The brain has to catch up with its new body image, food and diet changes, and sometimes chronic pain which has become a part of the new life. Often times, a person faces depression, fear and PTSD which causes sleep disturbances, and further delays mental healing.
Coming to terms with and accepting the new person post-surgery is an enormous and daunting hurdle. Having someone to speak with confidentially who can help to guide a patient through this process is essential. In addition, the caregivers in the equation cannot be neglected. They too have to come to terms with their new partner or spouse or loved one who is forever changed. Helping the caregiver to grapple with these changes is also much needed, as caregivers are many times the primary support system for an individual who has undergone major surgery.
Making a plan, setting long term goals, and then short-term goals that are achievable are important in achieving success with positive mental health. Speaking to a health care professional and understanding the importance of a support system including friends, family, and community are the pillars of a successful and positive mental health post-surgery, and recovery from PTSD due to major surgery.
References:
Dobson, G.P., Trauma of major surgery: A global problem that is not going away. International Journal of Surgery, 2020. 81(47-54).
Stanzel, A., Sierau, S. Pediatric Medical Traumatic Stress (PMTS) following Surgery in Childhood and Adolescence: a Systematic Review. Journ Child Adol Trauma 15, 795–809 (2022). https://doi.org/10.1007/s40653-021-00391-9